Keratoconus is characterized by the thinning and irregular steepening of the cornea, causing it to bulge outward into a cone-like shape. This structural change, in turn, leads to significant visual distortions, such as blurred and distorted vision, sensitivity to glare and light, and difficulty with night driving.
The underlying cause of keratoconus is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Researchers have identified several genetic mutations that may contribute to the development of the condition, and environmental factors like eye rubbing and chronic eye irritation can also play a role in the progression of keratoconus.
At the Khanna Vision Institute, our team of experienced ophthalmologists utilizes the latest diagnostic techniques, including corneal topography and aberrometry, to accurately assess the extent and severity of the corneal changes associated with keratoconus. This comprehensive evaluation allows us to develop personalized treatment plans that address the unique needs of each patient.
Pathology of Keratoconus
Thinning of the Corneal Stroma:
The most prominent feature of keratoconus is the thinning of the central and paracentral corneal stroma.
This thinning results in the characteristic conical shape of the cornea.
Collagen Fibril Abnormalities:
Disorganization and fragmentation of collagen fibrils in the corneal stroma are observed.
Changes in the collagen cross-linking result in weaker structural integrity.
Breaks in Bowman’s Layer:
Bowman’s layer, a tough layer between the epithelium and stroma, shows disruptions and breaks.
This contributes to the irregular surface and instability of the cornea.
Iron Deposits (Fleischer Rings):
Iron deposits can accumulate around the base of the cone, forming Fleischer rings.
These are visible upon slit-lamp examination and are indicative of the disease.
Epithelial Changes:
The corneal epithelium overlying the cone can become thinner.
Microcysts and epithelial plugs may also be observed.
Scarring:
In advanced stages, scarring may occur, further compromising vision.
This is due to the chronic mechanical stress and possibly minor ruptures within the corneal layers.
Biochemical and Cellular Changes
Increased Enzymatic Activity:
Elevated levels of proteolytic enzymes such as matrix metalloproteinases (MMPs) are found in keratoconic corneas.
These enzymes contribute to the degradation of the extracellular matrix and corneal thinning.
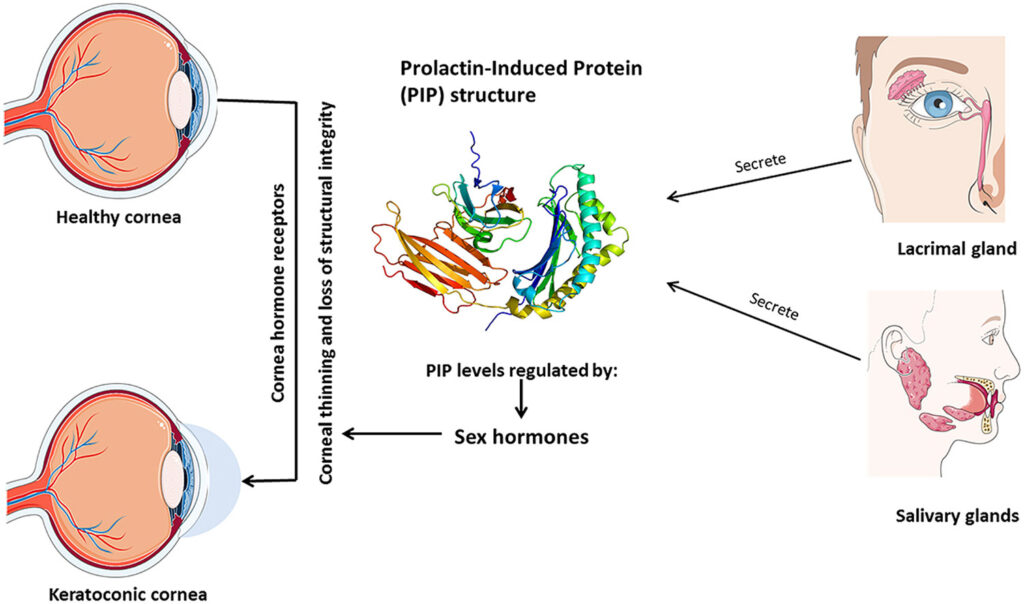
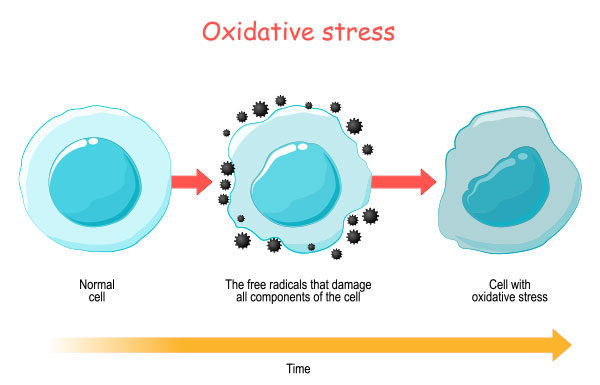
Oxidative Stress:
Increased oxidative stress and reduced antioxidant defenses are implicated in the pathogenesis of keratoconus.
Oxidative damage can lead to cellular apoptosis and weakening of the corneal structure.
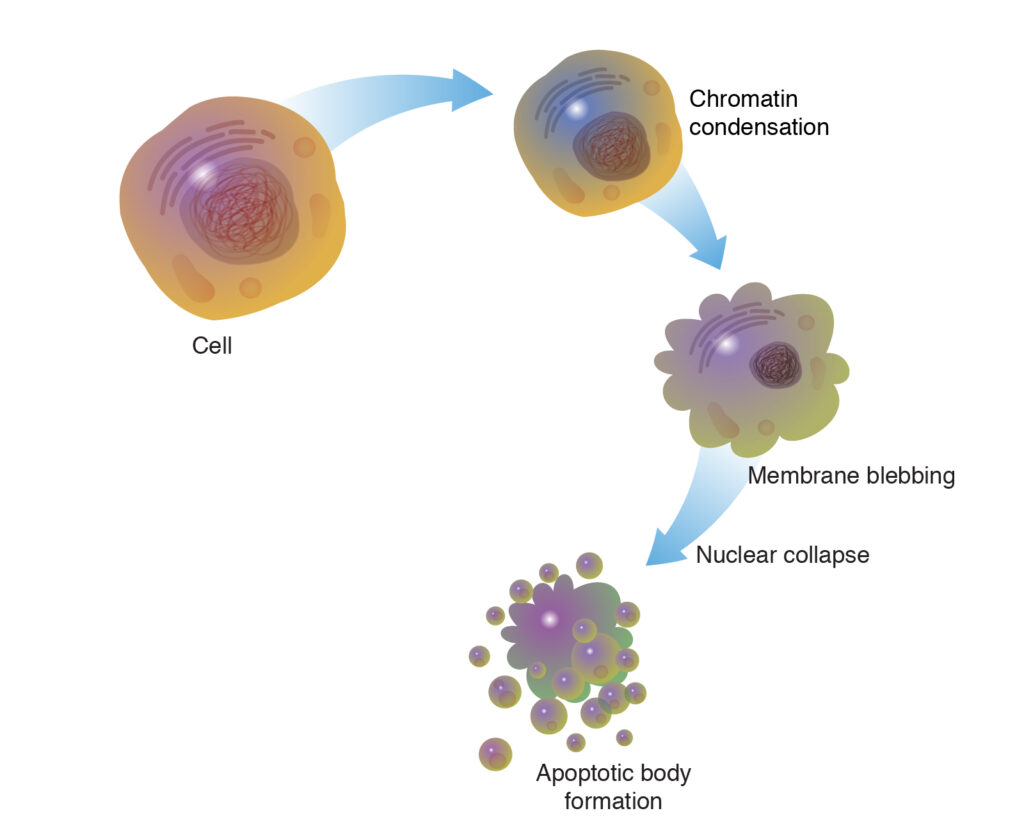
Cellular Apoptosis:
Increased apoptosis of stromal keratocytes (corneal cells) is observed.
This reduces the number of cells available to maintain the corneal matrix, contributing to thinning and weakening.
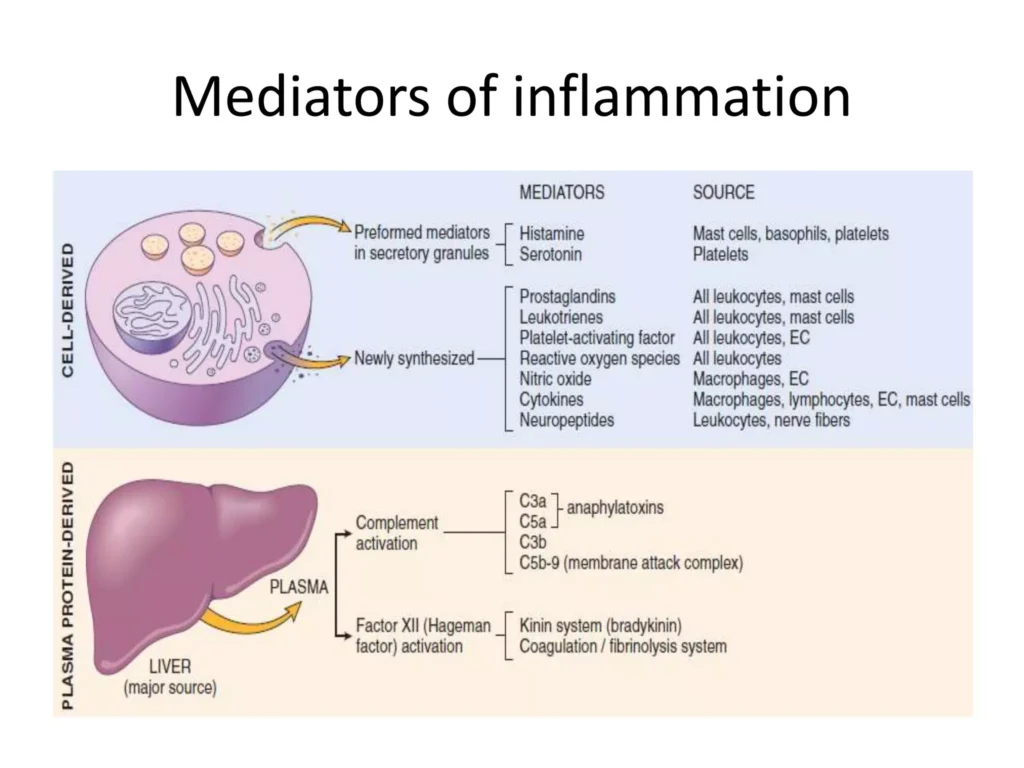
Inflammatory Mediators:
Although keratoconus is traditionally considered non-inflammatory, some studies have shown elevated levels of inflammatory cytokines.
This suggests that low-grade inflammation might play a role in the disease process.
Genetic Factors
Genetic Predisposition:
Keratoconus has a genetic component, with higher prevalence among first-degree relatives.
Multiple genes have been implicated, though no single causative gene has been identified.

Associated Genetic Syndromes:
Keratoconus is associated with certain genetic disorders such as Down syndrome, Ehlers-Danlos syndrome, and Marfan syndrome.
These associations suggest a genetic predisposition linked to connective tissue abnormalities.
Environmental and Mechanical Factors
Eye Rubbing:
Chronic and vigorous eye rubbing is a significant risk factor for keratoconus.
This mechanical trauma may exacerbate corneal thinning and progression of the disease.

Contact Lens Wear:
Poorly fitted contact lenses can cause chronic irritation and contribute to the mechanical stress on the cornea.

Ultraviolet (UV) Exposure:
UV radiation can induce oxidative stress, which might play a role in the pathogenesis of keratoconus.
By understanding the pathology of keratoconus, the Khanna Vision Institute is dedicated to providing our patients with the most effective and innovative treatments available, empowering them to manage their condition and maintain their visual acuity and quality of life.